This case is written by Dr. Donika Orlich. She is an Emergency physician practising in the Greater Toronto Area. She completed her Emergency Medicine training at McMaster University and also obtained a fellowship in simulation and medical education during her training.
Why it Matters
DKA is a reasonably common presentation to the ED. However, it requires several important steps in its management in order to prevent harm. This is especially true in children, where the rates of cerebral edema are higher. This case highlights several important features in the management of Pediatric DKA, including:
- That there is no role for an insulin bolus.
- That the precipitant of DKA must always be considered (in this case, it is appendicitis)
- That cerebral edema is a known complication of DKA and must be managed immediately with a reduction in the insulin and fluid rates as well as with either mannitol or hypertonic saline
We have previously published a case of Pediatric DKA on emsimcases. Today’s case is unique in that it begins with the learners providing advice over the phone to a physician who is less comfortable managing DKA. We have chosen to publish on this topic a second time as a way to emphasizes how cases on the same topic can be designed with different objectives in mind. The objectives (and therefore the case design) can lead to very different learning experiences. We have no doubt that this new case will also lead to excellent debriefing and evidence review with learners – it certainly does when we run it for our senior residents at McMaster University!
Case Summary
The learners receive a call from a peripheral hospital about transferring an unwell 8-year-old girl with new DKA. She has been incorrectly managed, receiving a 20cc/kg bolus for initial hypotension as well as an insulin bolus of 8 units (adult sliding scale dose for glucose of >20). The learner must perform a telephone consultation and dictate new orders. On arrival, EMS will state that they lost the IV en route, and the patient will become more somnolent in the ED. The learner should begin empiric treatment for likely cerebral edema and concurrently manage the DKA. Physical exam will show a peritonitic abdomen with guarding in the RLQ. Empiric Abx should be started for likely appendicitis. Due to decreasing neurologic status and vomiting, the patient will eventually require an advanced airway. The challenge is to optimize the peri-intubation course and ventilation to allow for compensation of her metabolic acidosis.
Clinical Vignette
Outside Patch: We have an 8-year-old female we want to send for DKA. She presented after feeling generally “unwell” for 3 days, with some accompanying abdominal pain and vomiting. Her blood glucose came back at 24 with a pH of 7.15 and HCO3 of 12, so we made the diagnosis of DKA. She received a 20mL/kg bolus for hypotension (BP 90/60) and Humulin R 8 unit bolus (as per our hospital sliding scale). What do you want for insulin and fluids before we send her?
Download the case here: Pediatric DKA
Post-intubation CXR for the case found here:
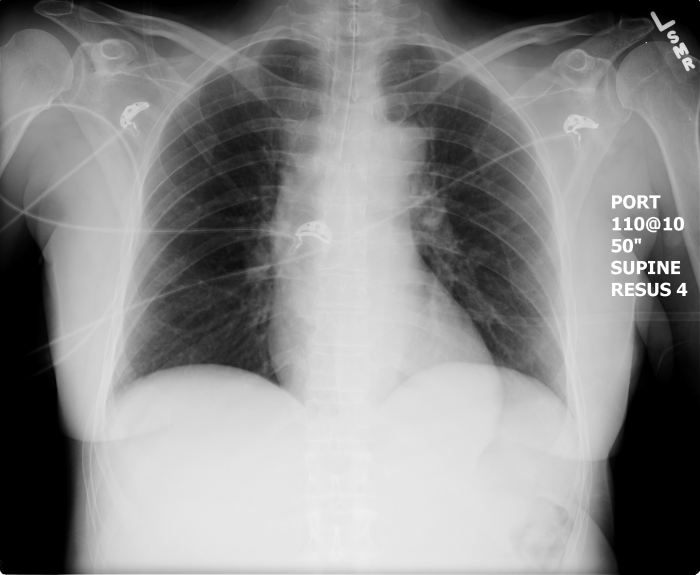
(CXR source: https://emcow.files.wordpress.com/2012/11/normal-intubation2.jpg)