This is the fourth COVID-19 case that we are publishing to provide simulation tools to healthcare providers during the 2020 COVID-19 pandemic. It involves an out of hospital cardiac arrest due to STEMI in a suspected COVID-19 positive patient.
This case was written by Trevor Campbell and Jared Baylis for use to assess and improve team preparedness to care for an incoming suspected COVID positive patient who has suffered an out-of-hospital cardiac arrest.
Why It Matters
Outbreaks of novel respiratory illnesses occur with some regularity (e.g. Severe Acute Respiratory Syndrome (SARS) and Middle-East Respiratory Syndrome (MERS)). With world travel being a modern reality, disease spread can happen quickly requiring careful infection control practices. COVID-19 (aka 2019-nCoV & SARS-CoV-2) was first detected in Wuhan, China in December 2019 and has since been declared a pandemic by the WHO (see this link for further information).
The COVID-19 worldwide pandemic has overwhelmed healthcare systems in many countries and led to catastrophic loss of life. Many healthcare providers have been exposed and infected in the course of their work and protocols to protect providers have been rapidly evolving. Simulation is being used to test and improve systems in place for infection control, PPE, and management of exposure to COVID-19.
This simulation case tests the response to an out-of-hospital cardiac arrest, and the ability of the staff to stay safe while caring for a critically ill patient. At the time of publishing, there is no unified, consensus approach to code blue in the suspected or confirmed COVID-19 patient. However, in this case, we explore an approach that maximizes the protection of healthcare providers and we encourage you to explore your local protocols in any simulation exercises you plan.
Clinical Vignette
Patient is currently being transported by advanced care paramedic crew, post VF arrest. Pt was found unresponsive by friend, immediate bystander CPR prior to EHS. EHS arrived and performed CPR. ROSC was obtained and the patient’s vitals afterwards were HR 110 sinus tachycardia, BP 80/60, no intrinsic respiratory effort, being ventilated with an iGel supraglottic device in place, GCS 3. ECG at the scene showed anterior ST elevation.
Case Summary
The patient is found by a friend unresponsive after a 7 day history of cough and shortness of breath. He immediately receives bystander CPR. An advanced care paramedic crew attends the scene and manages a ventricular fibrillation arrest prior to transporting to hospital. The patient goes into cardiac arrest again shortly before arriving in the emergency department. The team will need to prepare for the patient’s arrival and then manage a cardiac arrest using appropriate precautions for suspected COVID-19.
Download the case here: COVID OHCA
ECGs for the Case
Prehospital ECG:
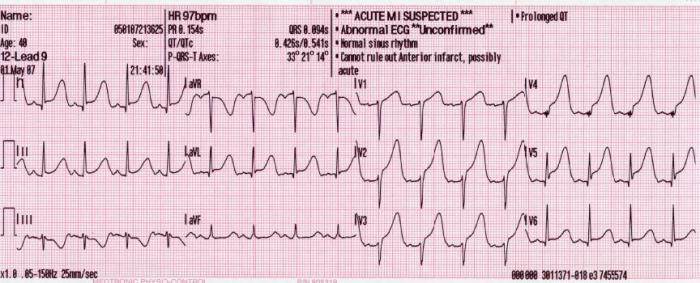
Source: https://commons.wikimedia.org/wiki/File:12_lead_generated_anterior_MI.JPG
ED ECG Post ROSC:

Source: https://en.wikipedia.org/wiki/File:12_Lead_EKG_ST_Elevation_tracing_only.jpg